Why Do I Wake Up with Dry Eyes? The COMPLETE Nighttime Guide
Waking up with dry, irritated eyes can make your mornings miserable — but it’s more common (and fixable) than you might think. This complete nighttime guide explains why your eyes dry out while you sleep, from eyelid gaps and sleep position to medical procedures and eye conditions. Learn how to identify the cause and what you can do tonight to wake up refreshed and comfortable again.
The Complete Guide to Dry Eyes: Why They Happen Overnight and During the Day (and How to Fix Them)
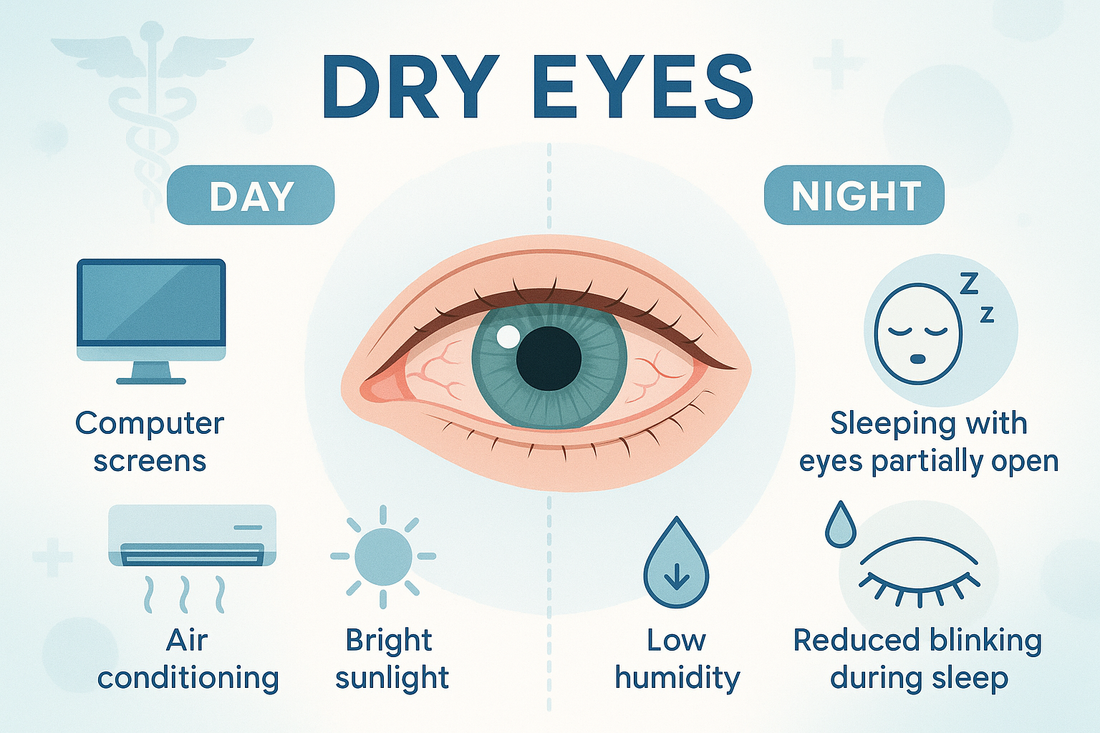
Dry eyes are more than just an annoyance — they can disrupt your mornings, your sleep, and even your ability to focus during the day. Millions of people wake up with burning, sandy eyes, while others find their eyes aching after hours on a screen. Both problems share a root cause: your eyes are losing moisture faster than they can keep it.
This guide is designed to be your one-stop resource for dry eyes, both at night and during the day. We’ll start with why mornings are such a problem, cover every major cause (from eyelid closure to CPAP machines), walk through the risks of ignoring it, and give you a step-by-step plan for lasting relief.
Table of Contents
- Why Do Eyes Feel Dry in the Morning?
-
Causes of Dry Eyes While Sleeping
A. Eyelid-Related Causes: Nocturnal Lagophthalmos
B. Post-Surgical Dryness (LASIK, Cataract, Eyelid Surgery)
C. CPAP Machines and Air Leaks
D. Environmental Dryness
E. Systemic and Lifestyle Factors
F. Vision Therapy or Strabismus Treatment - Risks of Ignoring Nighttime Dry Eyes
- Fixing Nighttime Dry Eyes: The Routine That Works
- Daytime Dry Eye: Why It Happens and What to Do
- Special Populations to Consider
- When to See a Professional
- The Most Comfortable Way to Protect Your Eyes Overnight
- Conclusion: Building Your Eye Oasis
- Sources & References
1. Why Do Eyes Feel Dry in the Morning?
At night, tear production drops by up to 70%. Normally, your eyelids act as a protective seal, trapping in what moisture remains. But if the lids don’t close completely, or if air circulates across your face, evaporation wins.
Other factors like low bedroom humidity, CPAP airflow, or surgery-related changes make the situation worse. That’s why so many people wake up with burning, gritty, or red eyes — a condition often called nighttime dry eye.
2. Causes of Dry Eyes While Sleeping
A) Eyelid-Related Causes: Nocturnal Lagophthalmos
When eyelids don’t fully close, even tiny gaps allow moisture to evaporate. This condition, called nocturnal lagophthalmos, is surprisingly common. Causes include:
- Weak eyelid muscles or mild facial nerve issues (e.g., palsy)
- Post-surgical stiffness after eyelid or facial surgery
- Natural aging that reduces eyelid tone
If your eyes look partly open when you sleep, or you always wake with irritation, this is a likely culprit.
B) Post-Surgical Dryness (LASIK, Cataract, Eyelid Surgery)
Eye surgeries often disrupt corneal nerves that regulate tear production. This can reduce blinking efficiency or lead to lid closure problems. Eyelid surgeries (blepharoplasty) may also change the way lids meet, leaving gaps.
Temporary dryness is common after LASIK or cataract surgery, but some patients develop long-term nighttime exposure if not protected.
C) CPAP Machines and Air Leaks
Sleep apnea patients using CPAP machines often wake with unusually dry eyes. That’s usually due to small air leaks near the mask that direct airflow toward the eyes. Hours of exposure dehydrate the corneal surface. A properly fitted mask, a humidifier, or protective eyelid seals can resolve this.
D) Environmental Dryness
Bedroom air quality matters. Fans, heaters, and A/C vents speed evaporation, especially when aimed at your face. Sleeping in low-humidity rooms (common in winter) makes dryness worse. Even your sleep position can play a role: side sleepers sometimes expose one eye more than the other.
E) Systemic and Lifestyle Factors
- Age-related tear reduction
- Autoimmune conditions (e.g., Sjögren’s syndrome, thyroid eye disease)
- Medications (antihistamines, antidepressants, decongestants)
- Evening alcohol or dehydration
All these factors make your eyes more vulnerable to nighttime dryness.
F) Vision Therapy or Strabismus Treatment
Patients undergoing patching therapy for amblyopia/strabismus often develop eyelid skin irritation from daily adhesive use. Overnight, this sensitive skin may not tolerate harsh tapes.
Gentle alternatives — like soft silicone-based eyelid tapes — keep the eye closed without damaging skin, making them ideal for people already under patching regimens.
3. Risks of Ignoring Nighttime Dry Eyes

- Corneal Abrasions: A dry corneal surface is fragile. Even your first blink can cause micro-scratches.
- Chronic Inflammation: Ongoing dryness triggers irritation and sensitivity to light, screens, or wind.
- Poor Sleep Quality: Discomfort can subtly pull you out of deep sleep cycles.
- Daytime Dryness: A destabilized tear film overnight often means you start the day behind, relying on artificial tears.
4. Fixing Nighttime Dry Eyes: The Routine That Works

Step 1 — Seal the Eyelids
- Use eyelid-specific tapes or shields to keep lids closed.
- Avoid medical/surgical tapes — they’re too harsh for eyelid skin.
- For severe dryness, moisture chamber goggles create a mini-humid environment.
- EyeOasis Sleeping Tape: designed specifically for overnight comfort, gentle removal, and no residue.
Step 2 — Add Overnight Lubrication
- Use preservative-free ointments or gels before bed.
- Apply 10–15 minutes before sleep to allow even spread.
- Avoid heavy overuse, which can blur vision into the morning.
Step 3 — Optimize Your Environment
- Run a humidifier in the bedroom.
- Avoid direct fans or vents near your bed.
- CPAP users: refit masks, check for leaks, or pair with eyelid seal protection.
Step 4 — Maintain Eyelid & Gland Health
- Gentle eyelid cleaning reduces bacteria/oil that destabilize tears.
- Warm compresses stimulate the meibomian glands, improving tear stability.
Step 5 — Stay Consistent
- Most people see relief within a week of nightly eyelid sealing + lubrication + environmental control. Stick with it.
5. Daytime Dry Eye: Why It Happens and What to Do

- Dry eye doesn’t stop when you wake up. Daytime triggers include:
- Screen time & reduced blinking: People blink up to 60% less while on devices.
- Office environments: Air conditioning, vents, and recycled air dry out eyes.
- Contact lenses: Especially in low humidity, they worsen evaporation.
- Outdoor factors: Wind, sun, and allergens all destabilize the tear film.
Solutions for Daytime Comfort
- Blink more often: Practice full blinks, especially on screens.
- Follow the 20-20-20 rule: Every 20 minutes, look at something 20 feet away for 20 seconds.
- Position screens slightly below eye level to encourage lids to cover more of the cornea.
- Artificial tears (preservative-free) during work hours.
- Protective eyewear (wraparound sunglasses outdoors).
- Diet & hydration: Omega-3s (fish, walnuts, flaxseed) and Vitamin A support tear film health.
6. Special Populations to Consider
- After Eye Surgery: Always protect lids during healing; confirm methods with your surgeon.
- CPAP Users: Control leaks and use eye protection if dryness persists.
- Strabismus or Amblyopia Therapy Patients: Use gentle, silicone-based eyelid tapes to reduce irritation.
- Older Adults: Age-related tear decline makes preventive nightly routines more important.
7. When to See a Professional
If home strategies aren’t working, consult an eye doctor. Persistent dryness may signal:
- Meibomian gland dysfunction
- Exposure keratopathy (cornea not fully protected)
- Autoimmune conditions
- Nerve-related sensitivity post-surgery
Professional treatments include:
- Prescription anti-inflammatory drops
- Tear-stimulating medication
- Punctal plugs to retain natural tears
- Specialty scleral lenses
8. The Most Comfortable Way to Protect Your Eyes Overnight
If you’re struggling with nighttime dryness, lagophthalmos, or CPAP-related eye irritation, finding a gentle and consistent way to keep your eyelids fully sealed makes the biggest difference. Many people try medical tape or bulky moisture goggles—but those often cause skin irritation, discomfort, or shift during sleep.
That’s exactly why we created EyeOasis Sleeping Tape — a soft, skin-friendly silicone tape designed specifically for overnight eyelid protection.

Why EyeOasis Sleeping Tape Works
- Gentle but secure: Uses a breathable, medical-grade silicone adhesive that keeps lids comfortably closed all night without pulling skin.
- Dermatologically tested: ISO 10993-5 & 10993-10 irritation and cytotoxicity certified, so it’s safe even for sensitive skin.
- Residue-free removal: The part we are most proud about... the material softens naturally by morning — peels away without pain, redness, or residue.
- Designed for comfort: Thin, flexible form conforms to any face shape, so you can sleep naturally without pressure or bulk.
-
Perfect for:
- Nocturnal lagophthalmos or partial eyelid closure
- CPAP or airflow-induced dryness
- Post-surgery recovery (with doctor approval)
- Patching/vision therapy patients needing gentle overnight closure
Thousands of people who used to wake up with burning, sandy eyes now sleep peacefully with EyeOasis — waking refreshed and hydrated instead of irritated.
Conclusion: Building Your Eye Oasis

Dry eyes — whether overnight or during the day — aren’t something you just have to tolerate. By sealing lids, optimizing your sleep environment, and building healthy daytime habits, most people can dramatically reduce irritation.
At EyeOasis, our mission is to make this easier. Our gentle eyelid-sealing tape was designed by someone who lived with lagophthalmos and dry-eye fatigue — and wanted a simple, skin-friendly solution.
Whether you’re waking up dry, struggling through workdays, or recovering from surgery, this guide should be your blueprint for lasting relief.
Sources & References
Nighttime Dry Eye Physiology
- Tornero P, et al. Sleep and Ocular Surface: The Impact of Sleep on Tear Secretion and Dry Eye Disease. Int J Mol Sci. 2023.
- Tsubota K, Nakamori K. Effects of Sleep Deprivation on the Ocular Surface. Ophthalmology. 1995.
Eyelid Closure & Lagophthalmos
- American Academy of Ophthalmology (AAO). Exposure Keratopathy: Diagnosis and Management. EyeNet Magazine.
- Harrison W, et al. Nocturnal Lagophthalmos and Sleep Quality in Dry Eye Disease. Cornea. 2018.
Post-Surgical Dryness
- De Paiva CS, et al. Dry Eye Post-LASIK: Mechanisms, Risk Factors, and Management. Cornea. 2006.
- Yu EY, et al. Dry Eye Following Cataract Surgery: Risk Factors and Outcomes. J Cataract Refract Surg. 2015.
CPAP and Airflow-Related Dryness
- Hayirci E, et al. Ocular Surface Problems in Patients Using Continuous Positive Airway Pressure. Sleep Med. 2012.
- Kadyan A, et al. Ocular Complications of CPAP Use in Obstructive Sleep Apnea. Eye. 2010.
Environmental & Lifestyle Factors
- Wolkoff P. Indoor Air Humidity and Dry Eye Symptoms. Indoor Air. 2018.
- Uchino M, et al. Impact of VDT Work on Dry Eye Symptoms. Am J Ophthalmol. 2008.
Vision Therapy & Patching-Related Skin Irritation
- Repka MX, et al. Compliance with Patching Therapy for Amblyopia. Arch Ophthalmol. 2002.
- Coulthard M, et al. Skin Reactions to Occlusion Patching for Amblyopia. Br J Ophthalmol. 2002.
Daytime Dry Eye & Screen Use
- Patel S, Henderson R, Bradley L. Effect of Visual Display Unit Use on Blink Rate and Tear Stability. Optom Vis Sci. 1991.
- Rosenfield M. Computer Vision Syndrome: A Review of Ocular Causes and Potential Treatments. Ophthalmic Physiol Opt. 2011.
Professional Management
- American Academy of Ophthalmology. Dry Eye Syndrome: Preferred Practice Pattern® Guidelines.
- Stapleton F, et al. TFOS DEWS II: Definition and Classification of Dry Eye. Ocul Surf. 2017.
